CRP as a cause of hypertension?
Feb 18, 2007 - 11:40:36 PM
, Reviewed by: Dr. Rashmi Yadav
|
|
|
"We have discovered that C-Reactive Protein (CRP) is not merely a marker of the risk of hypertension, it actually induces hypertension."
|
By UT Southwestern Medical Center,
[RxPG]
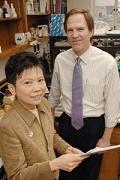 |
| Drs. Wanpen Vongpatanasin and Philip Shaul have discovered in mice that CRP is not merely a marker of the risk of hypertension, but plays a direct role in the onset of the condition. |
C-Reactive Protein, widely regarded as a risk factor for hypertension and other forms of cardiovascular disease, plays a direct role in the onset of hypertension, researchers at UT Southwestern Medical Center have found.
"We have discovered that C-Reactive Protein (CRP) is not merely a marker of the risk of hypertension, it actually induces hypertension," said Dr. Wanpen Vongpatanasin, associate professor of internal medicine and lead author of the study appearing in the February issue of Circulation.
UT Southwestern researchers studied mice with an engineered gene for CRP that was under the regulation of a second gene responsive to changes in dietary carbohydrate intake. The levels of circulating CRP, which is produced by the liver, were directly manipulated by altering the mice's diets, and the effect on blood pressure was determined. In this manner the actions of CRP were segregated from the actions of other mediators of inflammation.
"We found that when we switched on the gene that causes increases in CRP, the blood pressure went up, and when we turned off the gene and CRP levels went down, the blood pressure fell. Diet changes in the control mice had no effect, indicating that the blood pressure responses were due to CRP," said Dr. Vongpatanasin. "The cause of elevated blood pressure induced by CRP was also determined."
Clinical studies over the past decade have suggested that chronically elevated levels of CRP indicate inflammation that puts an individual at risk for hypertension and other cardiovascular ailments such as hardening of the arteries.
The mice in the latest study were supersensitive to angiotensin II, which is a major circulating factor regulating blood pressure via arterial constriction. This was due to alterations in key proteins in the vascular wall that are involved with angiotensin II.
Also, the researchers discovered that the initiating mechanism is a lack of the key signaling molecule nitric oxide in the artery wall, which has multiple beneficial roles in the cardiovascular system, as well as made a connection between nitric oxide and the proteins responsible for angiotensin II activity.
"Whether these same processes are operative in humans is yet to be determined," said Dr. Vongpatanasin. "We are also pursuing follow-up studies to further understand better how CRP causes the high blood pressure in the mice."
The ultimate goal of the research is to discover how CRP interacts with molecules in the artery wall, leading to a better understanding of hypertension and pointing to new ways to treat it, Dr. Vongpatanasin said.
"We have uncovered a series of mechanisms that link a circulating factor that rises with chronic inflammation, obesity and aging to the regulation of blood pressure," said Dr. Philip Shaul, professor of pediatrics at UT Southwestern and the study's senior author. "Doing so provides a new perspective on how these conditions have a negative impact on cardiovascular health."
Advertise in this space for $10 per month.
Contact us today.
|
 |
|
Subscribe to Hypertension Newsletter
|
|
|
|
About Dr. Rashmi Yadav
|
This news story has been reviewed by Dr. Rashmi Yadav before its publication on RxPG News website. Dr. Rashmi Yadav, MBBS, is a senior editor for RxPG News. In her position she is responsible for managing special correspondents and the surgery section of the website. Her areas of special interest include cardiothoracic surgery and interventional radiology.
RxPG News is committed to promotion and implementation of Evidence Based Medical Journalism in all channels of mass media including internet.
|
|
Additional information about the news article
|
Other UT Southwestern researchers involved in the study were Dr. Gail Thomas, associate professor of internal medicine, and Dr. Randall Schwartz, research fellow in pediatrics. Researchers from the University of Kentucky in Lexington and Case Western Reserve University School of Medicine also participated.
The study was supported by grants from the National Institutes of Health, the Donald W. Reynolds Cardiovascular Clinical Research Center, the Crystal Charity Ball Center for Pediatric Critical Care Research, and the Lowe Foundation.
About UT Southwestern Medical Center
UT Southwestern Medical Center, one of the premier medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. Its more than 1,400 full-time faculty members including four active Nobel Prize winners, more than any other medical school in the world are responsible for groundbreaking medical advances and are committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide medical care in 40 specialties to nearly 89,000 hospitalized patients and oversee 2.1 million outpatient visits a year.
|
|
Feedback
|
For any corrections of factual information, to contact the editors or to send
any medical news or health news press releases, use
feedback form
|
Top of Page
|



